A balanced approach
To maximize savings, we use:
- Medicare benchmarking
- Prospective inpatient claim review
- Negotiation
We assist in setting up Medicare benchmarking allowance as final out-of-network payment for high-volume, lower-dollar bills. Our prospective inpatient claim reviews and negotiation focus on:
- High-dollar billing errors and issues
- Duplicate charges
- Plan exclusionary denials
- Facility sign-off
Our experts assist in setting up a defensible out-of-network strategy that includes high-dollar and high-volume claims.
Network Solutions results
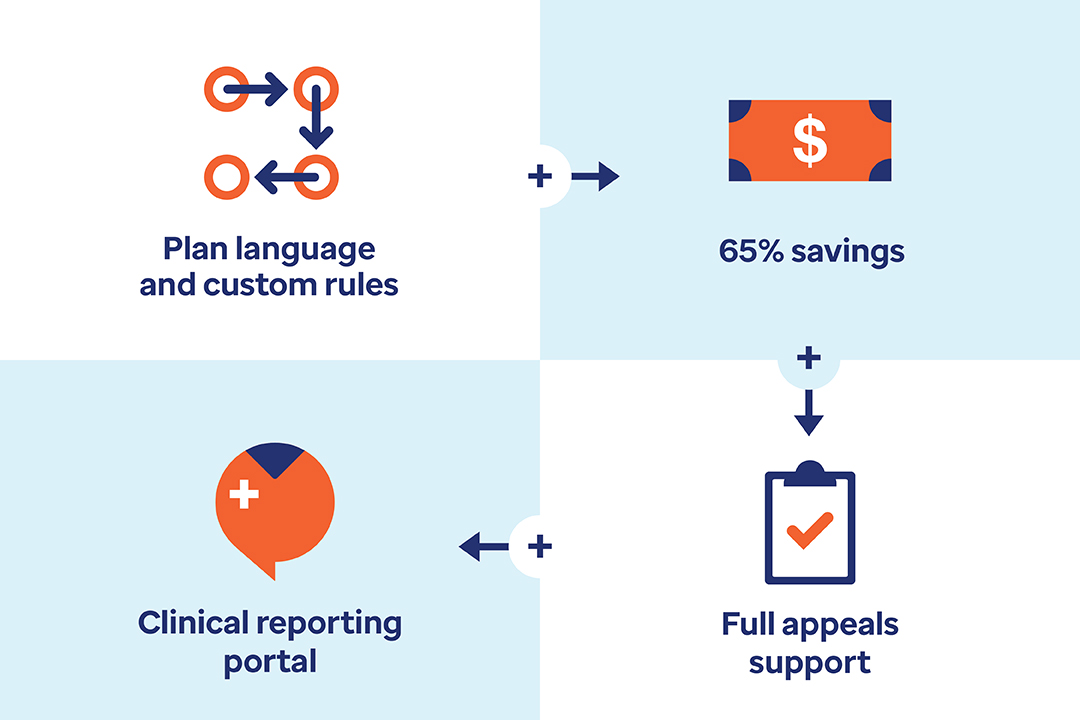
- 65% average savings of clients using a Medicare referenced-based position
- Over 90% uphold on appeals
How are our Network Solutions unique?
We ensure minimal provider abrasion with our consulting on plan language. We provide appeal support on all claims repriced, and a full-service report portal showing results.