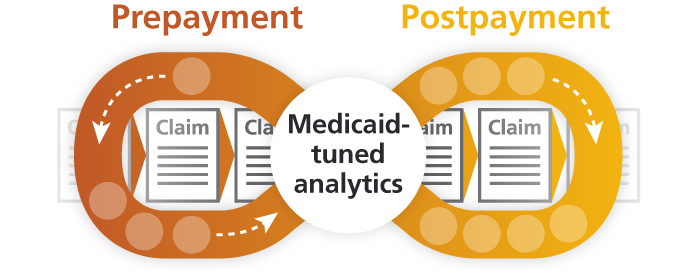
Optum® helps Medicaid agencies prevent, detect, investigate and recover improper payments throughout the claims cycle — from prepay to postpay. Our comprehensive program integrity suite is backed by experienced staff, saving Medicaid agencies millions of dollars each year.
Explore our solution
Advanced Communication Engine
Prevent claim inefficiency and lower administrative costs.



