Features

Improved transparency
Get access to robust provider metrics through executive and operational dashboards, providing a comprehensive view of your provider network. With insights into location, type, and enrollment status, states can better understand geographical gaps and identify communities that may be underserved and in need of additional Medicaid provider coverage.

Flexible integration
Compatible with existing modules, legacy systems, and third-party vendors, you can manage all provider types, organizations and atypical providers with ease. With over 100 configurations that allow for automated enrollment decisions, customizable instructions and more, Optum supports easier implementation into your current environment.

Enhanced administration for agencies
Our self-service gateway and support system simplify administrative activities, enhancing user experience and reducing total cost of ownership. The intuitive design ensures that agency staff can easily manage and monitor provider participation in Medicaid programs.

Reduced enrollment time
Dynamic screen workflows, up-to-date application status, easy-to use self-service capabilities and embedded tips & training reduce redundancies and speed up the enrollment process.

Ongoing assistance
From licensure and automated verification to simplified maintenance, we provide continuous support to ensure providers can focus on delivering quality care.
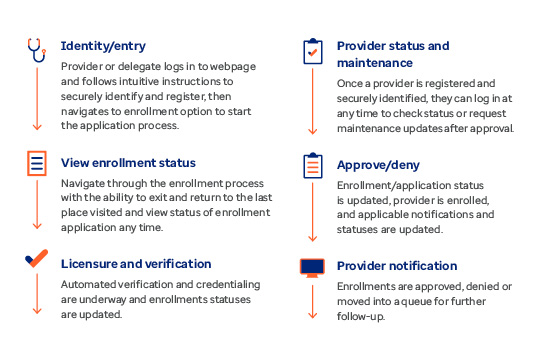
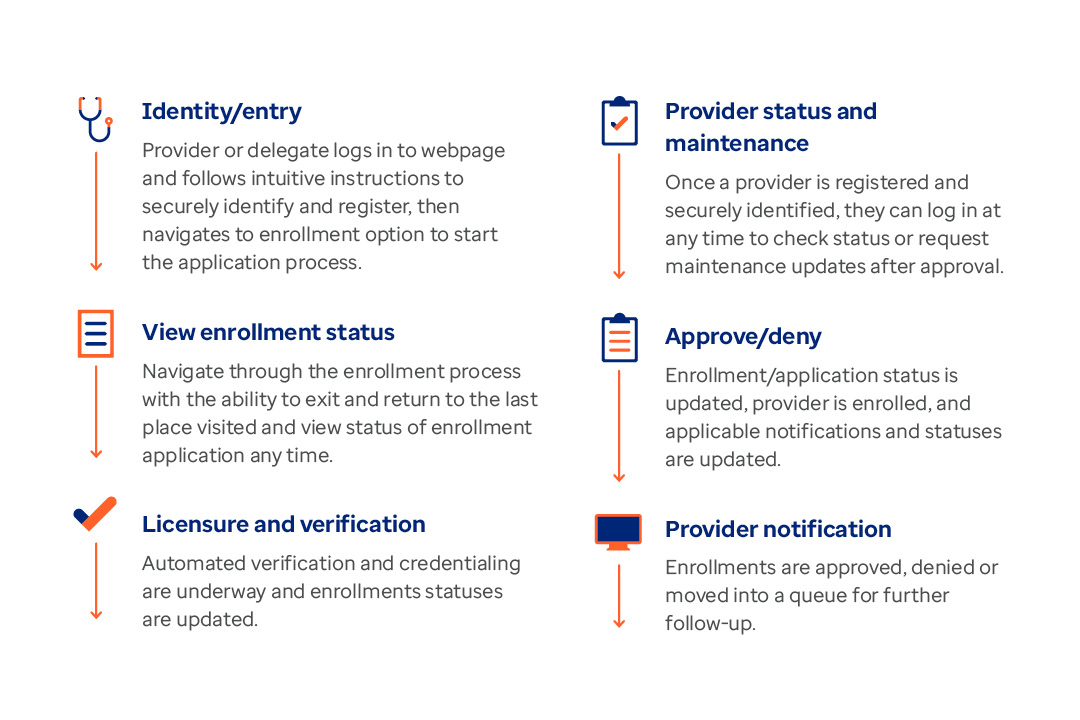
Provider enrollment workflow
Access a human-centered, intuitive online portal where providers can complete an application in as little as 20 minutes.
Choose a partner with experience
No other Medicaid Provider Management solution is built on the experience that Optum has in managing and operating provider networks.
- More than $120 billion net patient revenue managed on behalf of our partner hospitals and physicians' practices
- More than 90,000 aligned care delivery physicians across Optum Health
- Approximately 24,000 Advanced Practice Clinicians
- More than 300 Optum Care Ambulatory Surgery Care Centers (including SCA)
- More than 1,600 primary and specialty care clinics
- Approximately 2,470 Home and Community contracted skilled nursing home facilities
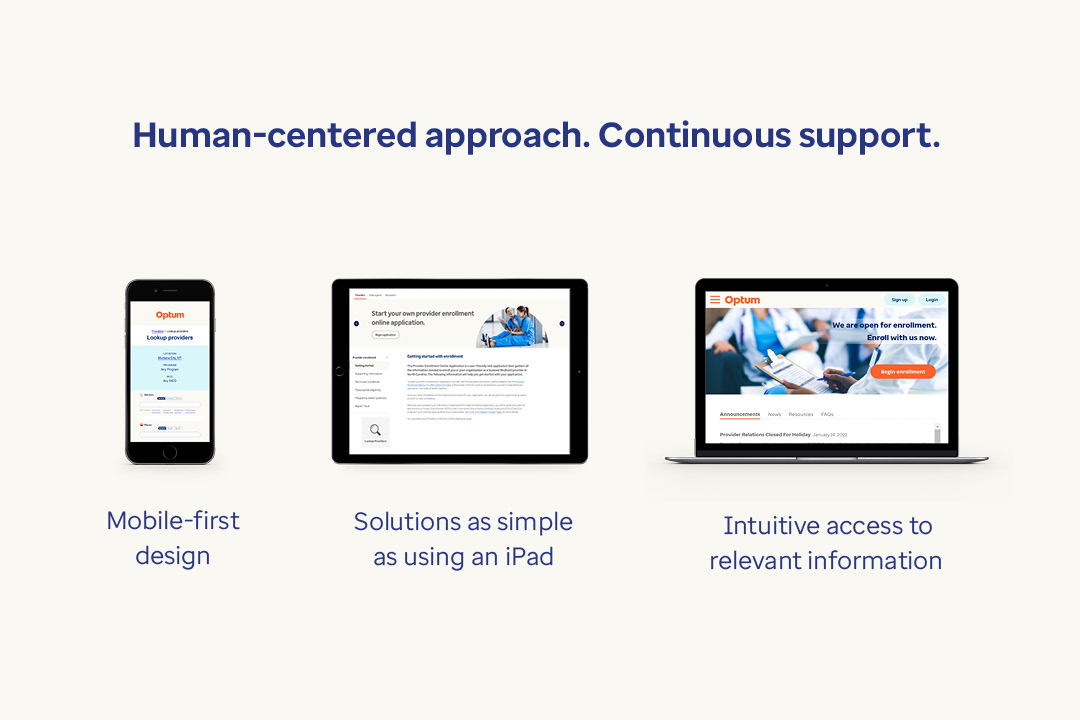
Continuous modernization for enhanced user adoption
Our mobile-first solution ensures easy access and a user-friendly experience on all devices. We’re committed to continuous improvements with regular updates to meet the evolving needs of provider enrollment and management.

Choose Optum as your NASPO ValuePoint vendor
Streamline your procurement process and save time with NASPO ValuePoint. Optum is a CMS pre-approved ValuePoint solution provider for the MMIS Provider Services Module. We provide our core provider management capabilities through ValuePoint’s cooperative procurement process, along with additional options for full-service management and enhanced self-service. We are here to support your agency every step of the way, ensuring you have the tools and support you need.
Visit our page on the ValuePoint website to view our Participating Addendum.