Features and Benefits
End-to-end solution
Our services-based solution offers end-to-end utilization management. It's backed by best practices in clinical staffing and workflows. The components of our solution include:
- Intake of provider requests
- Provider portal
- Technology platform
- Process workflows
- Automated decision software
- Utilization review by clinical staff
- Responses to providers
Reduced administrative burden for providers
Built on nationally recognized standards, our URAC-certified* solution creates efficient workflow and is easy for providers to use. Optum Utilization Management (UM) can automate determinations for certain procedures, delivering an immediate response to providers.
*Utilization Review Accreditation Commission
A positive provider experience
Our user-friendly portal is a single point of entry for Medicaid providers to submit prior authorization requests and receive fast responses. It also provides access for other Medicaid activities like claims submission and provider enrollment.

Recognized as leading to better outcomes
CMS has designated Optum UM as Quality Improvement Organization (QIO)-like for meeting rigid clinical standards for appropriate courses of treatment. QIO-like designation is important to states seeking Federal Financial Participation (FFP) for costs associated with medical and utilization reviews.

Near real-time reporting for operational efficiency
Near real-time operational reporting allows us to be more responsive to varying workloads. We can adjust clinical staff resources to facilitate faster determinations to providers.
Understand member and business needs
Optum UM aggregates member and claims data from multiple sources to analyze and quickly evaluate a member’s risk level. State agency staff have access to benefit determination records and reporting for aggregate analysis and case-by-case business need.
Flexible technology
We configure Optum UM to a state's specific Medicaid needs. This saves on the cost of customization. It is also interoperable with other MMIS modules and can work well as a stand-alone purchase for states.

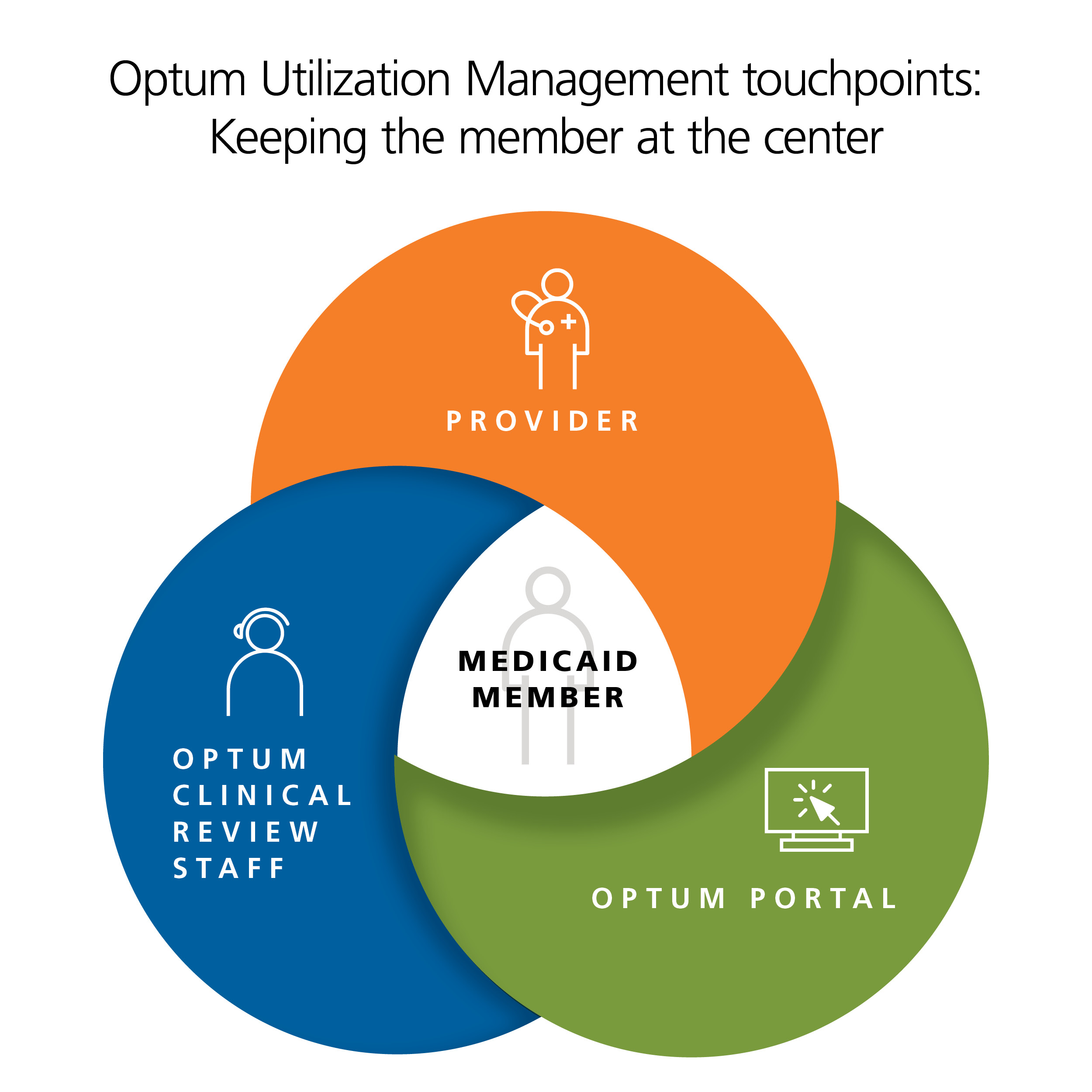
Balancing technology and human expertise
Our unique combination of technology and clinical expertise helps members receive the appropriate care as quickly as possible. With decades of experience managing population health, we know how to engage providers and members to achieve better health outcomes.



