A new approach to risk adjustment
Optum® Prospective Solutions offers pre-visit and point-of-care support to help improve member outcomes. Our services support early detection and ongoing evaluation of chronic conditions for Medicare Advantage (MA), Affordable Care Act (ACA) and Medicaid members on behalf of health plans. These services include:
- Prospective member assessments
- Digital integration strategy and implementation
- In-person and virtual support
- Member engagement campaigns
Meeting providers where they are
Optum works directly with providers to administer these services. We equip providers with actionable clinical insights, personalized member care gap information and administrative support. This helps create a workflow that prioritizes provider and member needs at the point of care and beyond. By reducing administrative burden, providers have more time to focus on clinical activities. In turn, this leads to better outcomes for members.
The Optum field team provides virtual and in-person support
The team is made up of 1,000 Health Care Advocates who work with 70,000 providers to manage 50 million gaps in care in all 50 states. They deliver wraparound services for providers that are customized to the level and type of support each practice requires.
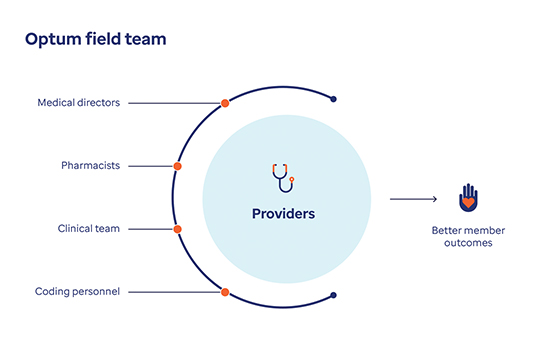
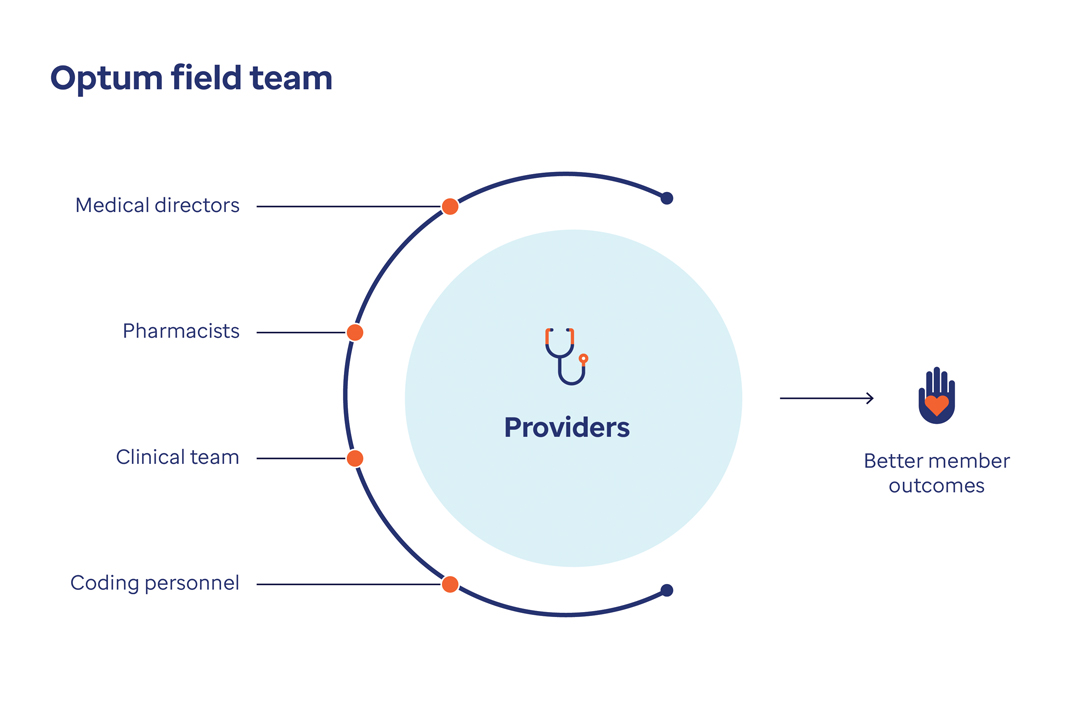
The Optum field team includes medical directors, pharmacists, the clinical team and personnel who help support providers. This support helps enable better member outcomes.
I have a caring relationship with my providers, we have the same goals … I’ve made an impact on the people I work with and they trust me.
Health Care Advocate, Optum
Cara Spahr
The time to be member-centric is now
We use predictive analytics to steer members with chronic conditions to their preferred modality of care and offer services that support whole-person care.


Activating members through multiple engagement levers
We follow up with members to schedule appointments, administer a social determinants of health (SDOH) survey, identify barriers and connect with resources.
Explore our solution
Fact sheet
Prospective Solutions fact sheet
Fact sheet
In-Office Assessment Program fact sheet
Case study
The Toledo Clinic case study
White paper
Help physicians spend more time with members
Help physicians focus on patients and spend less time on admin tasks.
Infographic
Engage providers to impact member outcomes
See how our field team can engage providers to impact member outcomes.
Executive summary
4 steps to optimizing value-based care
Take 4 steps to optimize value-based care with a holistic workflow.



