Webinar
A candid discussion on value-based care imperatives
Watch as Erik Johnson explores different risk models for delivering value-based care (VBC).
The right approach to VBC can help lower costs and improve patient satisfaction and care
Erik Johnson, senior vice president, Optum Advisory, recently hosted a webinar on value-based care (VBC) and key questions surrounding risk.

Video Transcript Title
- [Announcer] This meeting is being recorded.
- [Sherry] Hello, everyone. I'm Sherry Rohlfing, your host of the ACAP Value-Based Payment Showcase. ACAP presents periodic vendor showcases on a variety of topics so that our member health plans can hear directly from vendors on key services. Our next showcase will be in September, 2023, where vendors will be discussing social determinants of health offerings. Today, I'd like to walk you into our session presented by Optum and our presenter today is Erik Johnson. He will be presenting "Operating Imperatives for Value-Based Care." But before I turn it over, I have a few housekeeping items. This session, along with all ACAP calls and webinars will be held in accordance with the ACAP antitrust guidelines. These guidelines can be viewed on our website. We will record today's call and will post it and the slide deck on the Value-Based Purchasing Showcase website available to all of our member health plans. Always remember if your plan is seeking services, be sure to check out the list of preferred vendors on our website. Just look at the top of our homepage and click on the preferred vendor's link. When you're seeking services, you can also post a query or even an RFP on the Preferred Vendor Connection portal. During today's session, you can ask a question at any time by clicking the Q&A icon in your Zoom window and typing in your question. All questions will be answered during our session. Now I'll pass it over to Erik to kick it off.
- [Erik] Thanks, Sherry. Thanks very much and welcome to the webinar today. I'm Erik Johnson, I'm Senior Vice President at Optum Advisory Services. I run the value-based care practice here at Optum, and it's a pleasure to be speaking with you all today. For the next 45 minutes or so, we're gonna try to leave some time for Q&A at the end. We're gonna try to address some of the operational and functional demands that value-based care is putting on both payers and providers in the marketplace today. We're gonna talk a little bit about that in context about why value-based care, why now, what are the market imperatives in addition to the operating imperatives that payers and providers are facing in this ever-evolving market. So we'll talk a little bit about the models of EBC that are out there, the payment models that are out there, the partnership models that are out there, and really some of the strategic questions that folks are asking us as their consultants, but also asking of each other as different stakeholders in the marketplace today. As we go through this presentation, there's some questions I want folks to keep in mind that maybe will trigger some questions at the end. And feel free to ask these questions back to me as we get to the Q&A session later this morning, if I haven't addressed some of these in full. But we really wanted to bucket about four big sort of macro categories of questions. And the first is, in these payer provider arrangements, how close to first dollar premium risk do providers really want to be? Cause there's no single right answer for any particular stakeholder. Some folks will want to go to a full delegated capitation model in various product lines, whether that's Medicare, Medicaid or commercial. Some will only want to participate in upside downside ACO type models where there's a fairly narrow risk corridor, but they're still being rewarded for participating in a value-based care arrangement with particular emphasis on the quadruple aim. The next set of questions that folks I think need to answer or at least think about as they go down this route is, which populations should we be taking risk on? Because they all represent very different risk profiles. If you think about Medicare ACO populations versus Medicare Advantage populations versus managed Medicaid populations versus commercial populations, they all have very specific needs and you as a health system, you as a payer may be particularly well-positioned to take on one or two of those product lines, but maybe not all. So I think it's important to be intentional about the populations that we're targeting these value-based contracts on. As we think about value-based models and having providers take on greater responsibility, there does become an imperative for the providers to think about, do we have the necessary assets that we need in order to manage these populations? Do we have the right sites of care, the right care models, and the right primary care footprint in order to take on risk at scale with the populations that we choose to engage in value-based contracting? And then finally, and this is maybe just giving away a little bit of our mindset at Optum, we do think that these are largely partner-based models. We are generally not big fans of doing it all by yourself, whether that's owning all of the delivery assets that you need or whether it's starting your own provider sponsored health plan. In some cases, again, those may be the right answers, but in most cases what we have found is that is a big ask from a capital standpoint, from an organizational change standpoint and from a clinical standpoint. And so we very much think about this in terms of do you have the right partnerships in place in order to be successful in this endeavor? So that's kind of how we think about it. What I wanna get into now is sort of what are the fundamentals of value-based care? And I think a lot of us, at least I have been working in the world of VBC for about 15 years now, and the definitions have evolved. The marketplace has evolved. And I think if you ask 10 consultants what a good definition of value-based care is, you might get 11 different answers. So we think of it very much along the, what we were gonna cover in the next two slides. First of all, this is a contracting model. Value-based care ultimately is about value-based contracting. And that contract should include incentives that will enable a community partnership to make progress against the quadruple aim of lower costs, improved patient experience, improved provider experience, and higher quality. Now, there's some disagreement about this. Some folks have anchored very much on the triple aim, ignoring the provider satisfaction element of this. And some folks have extended this to the quintuple aim and included health equity in the equation. I think health equity is a good set of capabilities that may be appropriate for certain types of value-based care arrangements for certain types of populations. But in and of itself, health equity is almost too big of a lift to laden onto a value-based care contracting if it doesn't require those sets of capabilities. So we're very intentional about these four elements being represented in a value-based contract. And having those four elements in a VBC arrangement has some very specific implications. And we lay out four of those right here. The first is the implication for payment, moving away from that fee-for-service chassis, to something that is risk-based. Again, it doesn't necessarily have to be a capitated payment, it could be a risk-based fee-for-service model, like what we're seeing in the MSSP program across the country and what a lot of MA plans have adapted into their own arrangements with their provider networks. But we are looking to move towards risk and we will talk about the elements of risk in a minute. The second key implication is the implication for where that care is being delivered. And this is moving away from facility-based care as the primary delivery model and moving that care as close to home as possible. That is not to say we are arguing for a hospital-at-home model in every community or a SNF-at-home model in every community, but we are looking to move it into the community and out of the facilities to the degree that we can. The third implication is for risk management and who's gonna end up managing that risk? And in a value-based model, at least at a minimum, the risk management responsibility is shared between payer and providers. And in the most aggressive models, the risk management is delegated entirely to the provider network. And then finally, the implications for care design and delivery. And that is moving the payment model and the clinical model away from visit-based and episodic-based care models to longitudinal care models where instead of treating the episode, now you're treating the life or treating the patient or at least a year in the life of that patient for whom you have risk during that benefit period. And some of this may sound somewhat reductive to many of you, but I think it is important to keep in mind that all of these have to move in parallel as we look to find a sustainable value-based care contracting and delivery model for the partnerships involved. We talk a lot about risk in value-based contracting and there are four elements of risk in a VBC arrangement. And I think a lot of the attention is focused on that first one, that insurance risk, ultimately a value-based contract that includes insurance risk is an actuarial challenge, making sure that we have priced that risk correctly, that we've addressed the total cost of care even if we're still only operating in upside downside models where you're not on the hook for the entire total cost of care. That insurance risk has to be calculated. That insurance risk has to be shared. We have to come to some agreement that the provider network that is taking on some of that risk has an accurate understanding and complete visibility into how that insurance risk is calculated. And I think in a lot of cases, insurance risk is where a lot of the risk discussion stops, but there are other elements of risk in value-based contracting and I think they're largely accretive. I don't think you need to tread one off versus the other. In some cases you're gonna need all four. The second is quality risk and we're very familiar with that in the healthcare economy. CMS has been doing various elements of quality measurement and quality rewards and penalties for almost 20 years now through the inpatient hospital reporting mechanisms. And I think that is a good backstop to make sure that we are hitting our insurance risk goals without sacrificing our quality goals. The quality world is evolving fairly rapidly and expanding fairly rapidly to move beyond sort of the task list-based quality metrics that were the sort of first generation of quality measures moving into then outcomes-based measures, things like readmission penalties for hospital readmissions. And now we've extended beyond that into consumer and patient satisfaction. We've seen that in the MA program as the star rating regime starts to move away from what we would consider more of a HEDIS-based environment and more towards CAHPS and really getting at consumer satisfaction with their benefits and with their access points. That's quality risk. The third element could be operating risk, making sure that we're efficiently managing the anticipated demand by taking advantage of all of the sites of service available to the network and optimizing at the lowest cost, highest quality site of care and rewarding networks for managing those referral patterns intelligently. And then the last element of risk is what we call episodic risk. And that is managing episodes and procedures as efficiently as possible. This is an area where providers have had a lot of experience, roughly 40 years of experience to be precise since Medicare first introduced diagnosis-related groups back in the early eighties. Those diagnosis related groups, or DRGs, are really small bundled payments that really are meant to cover just the inpatient hospital stay. We have seen a lot of experimentation over the last 10 years with bundled payments. Certainly CMS invested quite a bit of time and energy in rolling out various models of bundle payments over the last decade or so with varying degrees of success. And I think there's a moment now where we're taking a little bit of a pause to see whether those types of episodic risk arrangements are sustainable in the long run. But certainly when you get into a full delegated model, there are certain types of providers you don't want to hold insurance risk, but you still want them accountable. We're talking about proceduralists and surgeons and subspecialties where they might not own a life during an entire 12-month benefit period, but they're gonna have a disproportionate impact on the amount of resources devoted to that life in a very discreet type of episode. And I think that's an important model to keep in mind as we go forward. So these are the various elements of risk that we include in risk-based contracting. These are the various elements that are largely present in accountable care models that CMS and CMMI have put forward through the MSSP program and now the ACO reach program, and I think all four of them are things that we need to think about and negotiate with our provider networks as we go forward. Now, as I mentioned at the beginning of the call, I've been working in value-based care for a better part of a decade and a half and it's always been the next big thing. And the question I think a lot of folks ask me now and that you may be getting asked as well is, "Why now?" And I think there are a couple reasons for that. The first is there are some significant macro headwinds facing the provider market today, which is making their business models that are based on fee-for-service increasingly difficult to maintain given the contracts that they have previously put in place. There are extraordinary inflation pressures across the healthcare economy. They're easing a bit over the last six months, but certainly the workforce shortages and supply chain disruptions that we've seen over the last 24 months have increased the operating cost basis for a lot of our healthcare providers in the last couple of years. We've also seen some pressures, some legislative and regulatory pressures on reimbursement and most recently on MA rates coming out from CMS. We've seen some market downturns in the stock market eroding some of the value of the endowments and cash reserves and liquid reserves that health systems have had in the past, which is further tightening their ability to operate with some latitude. And finally we see the expiration of the public health emergency a couple weeks ago, which is contributing to some dramatic swings in coverage through the Medicaid redeterminations that are ongoing and will be through the rest of the year, as well as some of the clawbacks from some of the waivers that providers have enjoyed since March of 2020. All of this is projected to put some significant downward pressure on provider operating income over the next few years. And I think that's an important consideration to have as provider systems and provider networks look to what is the next opportunity for margin in the market today. So those are sort of the macro economic dynamics that are forcing providers to think about value-based contracting as an alternative path to margin. But there are also sort what we would call endemic market disruptions that are happening to the provider market and that's been going on for quite a bit of time as well. We lay out a couple of those dynamics on this slide, on slide eight. The first dynamic that we call out for the purposes of today's discussion are what we would call the physician aggregators. These are the vendors that are going out, the Aledades and the Agilons and the Previews of the world who are going out and creating what are essentially synthetic IPAs with the idea of moving those into synthetic ACOs. And they are largely focused on the ambulatory market and on the independent practice groups that are still out there today giving them sort of purchasing power with payers in order to take on some of that risk and take on some of that delegator responsibility for populations primarily in Medicare Advantage today, but I think, increasingly moving into the commercial world as well. And in that dynamic what we see is a cutting out of the hospital as the middleman and the hospitals are struggling with the loss in volume from that. Second related trend is increasingly large physician practices scaling up to meet the VBC challenges that MA presents itself as an opportunity for top-line revenue growth and bottom-line margin improvement. About a fifth of physicians today are in large medical groups, what we would consider to be a hundred or more physicians and about 50% of Medicare release today are in MA products that those physician groups are targeting, again, threatening to cut out sort of the IDN health systems in the marketplace and also increasing their negotiating leverage with MA plans in their marketplaces. And finally, we have sort of the more consumer orientation that is happening in the marketplace today with the development of large ambulatory care centers of delivery. We see this with CVS and Walgreens in particular, making dramatic investments in their in-store clinics as well as the rising up of standalone urgent care centers. DMS has also contributed to this. There's about 115, 116 now hospital-at-home demonstration projects that are underway in various stages of maturity. All of this starting to really fundamentally change the course of the river of demand of healthcare services and forcing health systems, physician groups, specialty practices to think about what does the consumer journey look like today and can we manage that journey going forward with the existing assets that we have. So it's a very interesting time to be looking at the delivery, the market for the delivery of healthcare services given the macroeconomic challenges that folks are facing, which by nature are gonna be temporary and transient. But also looking at some of these more tectonic shifts in how healthcare is delivered and how healthcare is organized in local communities. It's creating urgency, in other words, for more and more providers to think more and more seriously about alternative contracting methods in order to make sure that they have sustainable business models going forward. And the way we've encouraged our payer and provider clients to think about this is that there are really two value levers in value-based care and it's where we start to see alignment between plans and providers and the first lever is growing market share in lives because we do believe value-based care is a growth strategy. It's not just an opportunity to take unnecessary utilization out of the system. It's an opportunity to grow the number of lives that we are responsible for as a partnership between plans and providers by providing more affordable products in the marketplace, richer benefit packages in the marketplace, and easier access to their benefits through the contracting mechanisms that payers put in place with their networks. Once you have all of those lives in those products, then the next challenge largely is to make sure that we're managing network integrity and driving demand into the select networks that we have put in place for those product lines. So what we call share of wallet to make sure that when there is necessary and required care to be delivered, that it is being delivered by our chosen network partners. Those are the value levers, those are the things that we measure. Then the next question is, are the enablers in place? And we'll talk more and more about the enablement factors in a couple of slides as we think about sort of how do you assess a provider network's capabilities for managing risk and managing populations at scale? But all of this applies to all of the different payment models that are out there today. And CMS, I have argued over the last 10 or 12 years, has been for better, for worse, the most creative and innovative payer that we see in the marketplace. They have tried more programs with more results with different types of providers than just about any other health plan out there, largely because they have the scale to do it and they have a congressional mandate to do it. And they started with upside-only MSSP models, rewarding networks who are able to manage utilization below certain thresholds without penalizing them for going over a pre-agreed upon benchmark. Those upside models still exist today in the MA and commercial world quite extensively in fact, and we tend to be relatively enthusiastic about upside-only risk models as a good point at which to start this type of investment campaign and this type of care model redesign. It gives providers practice at ingesting new sets of data, understanding how to analyze and model that data to identify opportunities for performance improvement and clinical utilization improvement. It gives payers who have adopted these models the ability to identify which provider networks are going to be good recipients of that claims data. Are they gonna be collaborative in generating new care models for the populations that are enrolled in those products? But it is in and of itself not an end game. And I think CMS is increasingly thinking about this as just a starting point, but moving more and more providers and more and more patients in the two-sided risk models. That's where we see a lot of the MSSP tracks today, presenting various levers and various models of upside and downside risk as well as the ACO reach model that they rolled out about a year ago. This is the first year live with that where they really are taking a fee-for-service chassis in Medicare and saying, okay, now we're gonna hold you pretty much at full risk for this population without fundamentally changing the benefit model and giving patients freedom of choice. It's a risky model, but it is sort of the natural evolution of where CMS has been taking the debate over the last decade or so. Now that's CMS, but what we continually advise our clients, our provider clients as well as our payer clients, is that for these models to work, it needs to work at scale. You need to be able to do it across as many of the populations that you serve. And that necessitates providers going to their plans in their marketplace to build upon the successes that they've had in those CMS programs and leverage those lessons learned into private contracting arrangements. You can do that by mimicking the CMS models upside downside risks and ACL models or depending on the maturity level that you've attained through those experiments, moving into full CAHPS risk arrangements with your payers in your marketplace. There's a wide plethora of payment models that are out there, but they essentially exist on this continuum. Now you've noticed, I haven't talked about bundled payments very much in these types of payment models. And that sort of does betray a little bit of our point of view on bundles. I think bundle payments can be a good tactic embedded in one of the four payment models you see at the bottom of this slide. But in and of itself, it's is not really a value-based care approach to a marketplace and that's because it is still largely dependent on volume and fee-for-service. And what we have found in certain markets is in both Medicare as well as in private pay bundle payment arrangements is that some provider networks are really good at managing bundles. They can make significant margin on particular types of bundles and then they end up doing more. So while they're optimizing their episodic risk performance, they're actually sub-performing on a total cost of care for a population standpoint because they're just doing more and more volume of things that they're really, really good at. So I think that's an important element of why we talked about operating risk as one of those four risk models that we're not overloading our specialty groups with too much volume simply because they're particularly efficient at a particular procedure. Talked a little bit earlier about growth and why this really is a growth model and we lay out a little bit of the math on this slide, attribution as a growth metric. I think this is sort of second nature for a lot of payers to think about growing the enrollment that they have in particular product lines. But it's a new model for a lot of providers out there in the marketplace and it really does require some education to think about attributable lives and what the opportunity is to grow your primary care footprint and the productivity of that primary care network. And I won't get too much into the details here, but what we have found is that there is significant productivity growth available in a lot of these primary care networks. They can certainly think about partnering beyond their existing owned or aligned primary care practices in order to have more exposure and more visibility into more lives. But what we see the real lift being is on that share of wallet capture. How much of the medical spend in that MOR is leaking out of the network and how much of that can we pull back? And that is going to be driven by how well you partner with the independent groups in a marketplace, how well designed those networks are and how well information is shared across those different practices and with the health system itself. That upside is going to be top-line revenue growth for most health systems with the proper contracts in place that can still represent an overall decrease in total cost of care for a given population. The trade-off there is in the denominator. Now what we're really looking to do here is grow the denominator so that the average per capita spend is lower, but you're doing it across a much broader population. That becomes immediately attractive to health plans who are looking to grow. And it becomes immediately attractive to health systems who can fundamentally execute against that referral management. And that's where incentives start to align and that's where you can really build some very interesting partnerships between payers and partners, payers and providers, and start to contract and memorialize those agreements in those contracts. Those contracts then need to really talk about four big things in order for this to work and the first is those contracting models. Have we gotten a risk correct? Is the revenue diversification something that we can live with and does it give everybody the best chance to grow in attributed lives and share of wallet? Then the next question is, are we giving our beneficiaries the tools that they need in order to access their benefits most effectively? And this is kind of a new dynamic that we have seen emerge with payers over the last three years and I think we saw the seeds of this planted during the summer of 2020, about four months into the public health emergency, health plans were in very good shape. People were not going in for elective care. There wasn't a lot of unnecessary demand in the healthcare system at that point in time. But I think gradually, very, very quickly health plans realized that at some point those individuals who were not seeking care were not just those who were avoiding elective care, they were individuals who were scared about coming in but had real chronic healthcare needs. And at some point they would come back into the system and they were gonna be much more expensive and much sicker than they would've otherwise had been if they'd been able to maintain their care regimes. So plans got pretty smart in some respects and in many markets about reaching out to those rising risks and identified risk populations to keep them engaged with their benefits, to keep them engaged with their providers. And what we saw was a lot of collaboration between health plans and their networks to make sure that those at-risk populations were able to maintain their health during a time of great uncertainty and their ability to physically access a physician office or an emergency room. Those are good lessons to have learned during the pandemic and I don't think that they were limited to the pandemic. They are lessons that we should mature and integrate into the way we think about benefit design and patient access and beneficiary access going forward. 'Cause what we have found in a lot of the engagements that we have done in Optum Advisory is that the more you can get those patients to engage with their benefits in a predictable way that leaves them satisfied with the experience, is that you also end up with better outcomes and lower total cost of care. And then finally, I think, what what we're looking to do in a lot of these joint contract payer provider partnerships is to memorialize some of these new care models and make sure that those care models are jointly designed by partnerships in place and that some of the ongoing care management functions are delegated down to providers. This is where I normally tell a quick story about sitting on a panel a few years ago with a representative from a large national carrier, a representative of a physician group. And I was representing health systems on that panel and it had nothing to do with what I said, but it had something to do with what the representative of a national insurance carrier said, which was that we hate risk as payers. We really hate the idea of having to manage risk. And I remember sitting in that panel thinking, well, that's why insurance companies exist is to manage risk. So I was a little befuddled by the statement and afterwards, I asked him what he actually meant by that statement. And he said, health plans are great at pricing risk. We have tremendous actuarial assets that can help us price that risk for beneficiaries, but we can't manage risk because we have beneficiaries and risk is managed at the patient level. And he wasn't trying to make a needless semantic distinction. I think he was making very meaningful distinction, that risk is managed at the patient level, that patient, the most direct relationship that will inflect that patient's behavior is with the provider. And we need to do a better job of delegating down to those providers, utilization management, care management, prior auth decision making and functions that have normally existed at the payer level but that we have historically struggled in doing a good job with. To a certain degree, we could help price that risk correctly, but then delegate the responsibility for managing it down to providers. And for that, new care models should be memorialized in those contracts. So that gets us to sort of our structure and our maturity model for value-based care. And I think this applies to all of the partnerships that we think about. The first is on your strategy, and we're really looking to answer three questions there. One is, who do you want to take risk on? Medicare, Medicaid, commercial? How much risk do you want to take? Upside-only, upside downside or full capitation? And third, who are you gonna partner with to go into this market with this new type of contract? What's your governance model going forward? Once you've established that North Star, then the next question is who's gonna go on that journey with you? And that's the network build and management function that you see on the top left there. I'm not necessarily just talking about clinically integrated networks here. I'm talking about a network that is sufficient to treat the patients that you have. And I know that sounds somewhat reductive, but if you think about Medicare Advantage or Medicare ACO populations, that network is gonna have to include skilled nursing and home health facilities that do more than just meet rate requirements. There are high quality skilled nursing and home health agencies who can manage populations on the extended tail of a post-discharge admission. It's gonna look different in Medicaid and it's gonna look different in commercial, but whatever it is. And then you can do all three. Those networks have to be bespoke to those populations. The next question is, what are you gonna ask them to do differently from a population health management and coding perspective? Are the care models and the care transition programs being put in place sufficient and scalable enough on the provider side to manage the volume that those populations are going to represent? And this requires a lot of change management both at the practice level as well as at the inpatient point of care as well. You're still gonna have a lot of necessary care. And so we wanna make sure that we're getting that operational episodic risk right through improvements in our care delivery. It's still gonna matter that we manage length of stay in all institutional settings effectively. It's still gonna matter that we take advantage of site of service arbitrage across all of our populations. All of that is gonna sit on an data analytics and reporting platform that ingest the right level of data with the right cadence and produces the right level of granularity for decision makers at the provider level to make decisions about where performance improvement initiatives need to take place. And finally, we wanna make sure that the enterprise risk is appropriately priced. And that is something that providers have very little experience in, payers have a great deal of experience in, and we wanna make sure that there's a new equilibrium established repairs and providers to jointly negotiate what that risk needs to look like. This is a long-term strategy and I won't get into the ones on the side, the enterprise governance, organizational commitment and change management because that's its own webinar. But what we're really talking about here from a value-based care standpoint is patients. We need these new partnerships to have a three to five-year point of view on this new opportunity. These are not basic payoff in 12 months. It does require sort of a multi-year and in many cases a multi-product line approach under a single infrastructure that the payer and provider partners have decided to erect around their communities and around the different populations that live in those communities. But it really does require folks to take that three to five year point of view. We'll talk about a couple opportunities here that are probably top of mind for a lot of folks. And the first is the Medicare imperatives. And I'm sure many of you're already familiar with this, but Medicare Advantage is insanely popular. Medicare Advantage is taking most of the growth and the over 65 population today. These are a few MSAs that we've charted out to show just how popular Medicare Advantage has become over the last few years. And this is true largely across the country. And I don't really see that waning anytime soon. CMS has a couple key priorities that they're constantly trying to achieve. The first is protecting the Medicare trust funds. and the second is making sure that their beneficiaries are happy. And Medicare Advantage is extremely popular for any number of reasons that I'm sure many of you are more familiar with than me. But this is the direction of travel for the over 65 population. And for providers who are seeing more and more of their volume represented by the over 65 population, they have to have a new approach to that population in order to make the economic models work for them. And there are really three ways to make these economic models work. It is to make those MA products more profitable for the plans that sponsor them and on whose licenses these products ride. And the first is to get accurate patient coding in place. Now I realize that there's a lot of discussion around how HCC scores are calculated and will be calculated going forward over the next three years. It's not going away, but it will be constrained a little bit by some of the decisions CMS is making. Nevertheless, for provider networks to show value, they have to be able to show in part that they're good at coding the visits that they get. The second is your total cost of care and your star ratings. Are the providers in the network providing the necessary level of population health that you can bring down total cost of care? And are they providing a consumer experience that will help the plan achieve the maximum level of star ratings in this new regime, which is largely based on consumer satisfaction. And then finally, is this a high-value network? Back to some of the capabilities we talked about in the maturity model. Is this a network that is relatively seamless, operates as a network, has fairly seamless referral patterns and provides the provider network itself its share of gains in demand? So we're minimizing that leakage. Increasingly the payer clients that we work with, that's really what they're looking for from their networks. And I think that's largely new. A lot of this is largely new to the networks that we work with on the provider side of the shop. That model is probably gonna sustain itself going forward, but there's a lot of pressure on that model going forward. And we lay out some of those pressures here and we've talked about most of these over the last 40 minutes or so. The expiration of some of the pandemic-related rating adjustments going away this year, it's gonna make star ratings a whole lot harder. Only about 51% of MA plans have a star rating of four or more this year. That that's down significantly from 2022. And that's largely because of the change, the ongoing change towards a more CAHPS-focused survey Medicare beneficiaries. But also because of some of the expiration of the pandemic relief that Congress put in place in 2020. This heightened focus on health equity is becoming a really interesting challenge for MA plans as well as providers to start to grapple with. Health equity is still a relatively new dynamic that is creating some uncertainty and some disequilibrium in these partnerships to try to figure out how to address it most effectively. I think there's a lot of innovation happening in this world and I encourage it and I think that there should be ongoing innovation in this because I don't think right now there is a right answer in how to approach the inequities that we see in our communities. I think there's a lot of experimentation and innovation happening, but I don't think we're to a new equilibrium in how we incorporate that into our benefit models and into our network designs. We've talked about the narrowing opportunities in coding that CMS rolled out in their advanced notice earlier in the spring and then in the final notice last month. This is gonna put pressure on top-line revenue opportunities for MA plans as well as for those taking delegated full CAHPS arrangements from MA plans on the provider side. It hasn't completely eliminated it, but I think it is going to change the points of emphasis away from top-line revenue growth, more toward managing total cost of care and really starting to get at some of that previously unaddressed, unanticipated and unnecessary demand. And finally, we've talked about CAHPS surveys. All of this requires some partnership. I don't think a payer is gonna be able to do this on their own and I don't think a provider network is gonna be able to do it on its own. It's gonna require the combined thinking and the combined insights from both sides of that equation in order to come up with sustainable solutions to this challenge. And I think it's worth coming up with an approach, a joint approach to this because for providers, MA is really the only place left for them to find margin in the Medicare population. Right now, they basically break even on Medicare populations and they basically break even on Medicare Advantage contracts, whereas all of the value right now, all of the excess value or all of the margin is focused on the provider, around 8% to 10% margin, for most of the payers that we work with. In order to grow, we think MA plans are gonna have to be willing to sacrifice some of that margin down to providers in order to grow membership. There is no other place for providers to get that. There is in the commercial world and that's largely where we've seen providers make money over the last few years. But given some of the challenges that we have seen in site of service reallocation, some of those disruptive tectonic trends that we talked about earlier. This is becoming less and less available to most health systems as they are starting to feel themselves marginalized by some of the new market entrants. So they are gonna have to double down on their Medicare Advantage bets and they're gonna have to double down on the discussions that they have with their community health plans in order to make sure that everybody can grow in a way that is sustainable going forward. That's the Medicare challenge. Medicaid opportunity is a little bit different. And in some respects from an analytic point of view, much more interesting in some respects because these populations have such heterogeneous needs going forward. And it is so difficult to keep these lives long enough for some of these population health investments that you make in these communities to really take hold and generate a positive ROI. But we have seen that it can be done. We have seen in our experience, at least within Optum Advisory, we have seen plenty of Medicaid managed care plans, provider sponsored Medicaid managed care plans really succeed in their ability to deliver high quality care to their communities as well as make some some top-line revenues and bottom-line margin. But to do that, they've had to become very aggressive in a couple of areas. One is to get very aggressive in their approach to analytics to understand what are some of the underlying trends in the Medicaid populations that might hide something that is gonna come back in later years and start to really affect their ability to make margin on those delegated arrangements. And the second area of major investment is investing in the community. And this is where Medicaid is really quite different from other VBC arrangements is that emphasis on community assets that can address these populations in place and address some of their social determinants of health in an effective way. Medicare Advantage, I think, the playbook there is pretty straightforward. We talked about some of those elements a few minutes ago. In Medicaid, what we have seen work and this slide comes to us from our sister company, the Advisory Board, and I think they've done a really nice job here of identifying some of the community resources that they have seen in their best practice research, certainly that we have seen in our consulting engagements, that overemphasis that over indexing on community health workers, clinical social workers, behavioral health and social determinant analytics. That is really gonna provide much greater access and insight into the needs of those populations, which is very different from a fully insured commercial life and very different from a fully insured Medicare Advantage life in general. One example I'll give you, we had a health system client that was taking delegated risk on Medicaid and they articulated to us what they called the $20 problem. They operated and served a community that had very little in the way of public transportation and those folks may be in the Medicaid managed care arrangement and after they left the hospital, they faced this $20 dilemma because after they left the hospital, they were prescribed a drug or a suite of drugs and they were scheduled for a follow-up visit with their primary care physician. But that patient, that beneficiary could really only afford one of those two options. They could either get an Uber to CVS or they could get an Uber to their physician practice, but they probably couldn't do both in a timely enough way. So the investment there was to determine from a community health worker perspective, let's go identify those who have transportation needs and then let's just provide the transportation to the beneficiary. It's easy enough to spend $20 on the Lyft ride or the Uber ride if what we're doing is getting that person compliant with their medication regimen and mitigating the risk that they're gonna have a flare up or an emergency room visit later that's gonna cost thousands of dollars. That's a trade off that they were willing to make. And that's not the most necessarily creative arrangement, but it is a little bit of that outside-of-the-box thinking that you can only get when you have community health workers in the community assessing for social determinants and then coming up with an actual cost effective solution to it going forward. That's the investment in the community. The investment in analytics. We talked a little bit about here and I'm gonna sort of wrap up here so we spend some time on Q&A. Same client, looking at sort of trend lines over time. And in aggregate, the trend lines were pretty good. What the trendline analytics were hiding were two things. One was catastrophic expense amongst a population. That's in that sort of that middle row there, you see that 24.3% non-chronic decline. That's decline in their MOR. These non-chronic folks who had catastrophic events, whether those were accidents or organ transplants, that's hidden in the trendline numbers. When that trendline reverses and the catastrophic events decline over time. What they end up finding is almost a 20% annual increase in spending on chronic care conditions, asthma, diabetes, CHF and COPD, in particular, that you see down there on the bottom right. They needed to understand how much catastrophic expense was either masking or outperforming their ongoing chronic trend spend line. And until they were able to get at that level of granularity and identify those patients with asthma, diabetes, CHF and COPD, they were unable to figure out where to invest their population health programs going forward. This is a level of granularity in the analytics that is available through the claims data, if you know and can commit enough time to really getting down to that level of care and understanding of the populations. That in Medicaid, that's where we spend a great deal of time working on these Medicaid value-based care arrangements, figuring out the community needs and making sure that the analytics are flying at the right altitude to provide us the understanding that we need in order to understand where we might be vulnerable in the next six to 12 months. So with that in mind, I think we get you right about 10 minutes to the top of the hour. I'm just back to the questions that I sort of proposed at the top of the discussion here. How close to first off premium risk do we want our providers to be? For which populations? In which types of partnerships? And what kind of assets are we gonna need to develop as part of that partnership in order to successfully manage that level of risk with that level of population? And with that, I think I might turn it over to Sherry to facilitate any Q&A.
- [Sherry] Thanks, Erik. We do have a few questions. The first one is, what role, if any, do you see for Pharma as a part of these models? Is it an outcomes-based contracting or payers and providers open to partnerships with Pharma that extend beyond that into health equity for, et cetera?
- [Erik] Health equity is the first frontier I think for Pharma partnerships in these models. I think certainly, we've seen some sort of innovative contracting to address some of the social determinants for the Medicaid population in particular. I think outcomes-based contracts are really interesting in this realm. And I'll be honest, I'm not quite sure that outcomes-based contracts have gotten a level of maturity that we know what the best practices there are, but I think there's a lot of attention spent on pharmaceutical pricing and I think that's certainly nothing that we can ignore in these contracts. But I also think that there's an access issue that we're probably missing with a lot of our at risk populations. And I think being able to reconcile the medication regimes that they're on, making sure that they have access through discounting programs and the like and the ability to manage the outcomes of those populations, it goes beyond sort of the pharmaceutical contract and gets into what does that contract mean for what the physician practices and the physician extenders need to do in order to follow up once those scripts are filled. I think it's largely been approached as sort of a bilateral equation to solve between the pharmaceutical company and the risk bearer. I think it's a little bit more multidimensional than that. We have to sort of tease out what that's gonna mean for physician follow up, physician extend or follow up to make sure that the patients are taking the drugs the way that they need to. And I think pharmaceutical companies, at least in my limited experience with Pharma, is that they have good ideas about how to engage the provider networks to make those contracts as valuable as possible. But I think it's early days, I think it's very early days in figuring out what best practice there is.
- [Sherry] Okay, we do have a couple other questions. How is the lack of data available impacting things and what can be done to improve it?
- [Erik] Yeah, I get that question a lot. There isn't a lack of data. There's a lot of data in healthcare as everybody is aware. And I think we're sort of past this as an industry, but I think it's relatively recent that people were waiting for complete data sets. We want clinical, we want claims, we want social determinants, we want it all before we can do anything. And I think we're largely past that. I think claims data in and of itself can tell you a lot. Now there's a latency to that, that I acknowledge, and if you're looking to do real time performance improvement, claims data is not gonna be a sufficient data set for you to use. But if you're doing long-term planning and trying to figure out an analytical basis on which to base the investment decisions that you make, certainly from a health perspective, claims data can give you a lot. I think the challenge has been making sure that data is shared with the provider networks that you're asking to perform either in a value-based contract or not. I think providers would tell you, health systems would tell you that they don't have enough access to the claims data for the populations that they serve. And that is more of a legal and negotiating question than it is whether there's oil in the ground. There's plenty of oil in the ground to be drilled, but you need to have those contracts in place that enable both parties to be able to take advantage of that asset. I think now we're in a world where we're starting to integrate clinical data with that claims data, which can produce more real time data for sure if we can aggregate it and model it effectively to drive maybe near real time performance improvement. But there are all sorts of questions about sharing that data back with the payers because the providers can own the clinical data. So again, there's plenty of data assets out there that can provide, properly modeled, the right level of insight into the populations that you serve. It's just a question of sitting down and making sure that both parties are getting what they need out of it. That's the first order challenge. I think the second order challenge is making sure that you have the ability and the resources in-house or through a third party to model the data in a way that is useful and will tell you something. One of the things that we have found is that there's plenty of data reporting, but that data reporting is serving sort of very discreet financial needs and when shared with clinicians, with physician groups and with practices, it doesn't really give them much to act on. And I think modeling it in such a way and getting that modeled data out to those physician practices in a way that they can actually use it, that's the real art of all of this and that requires some change management on the part of the physician groups.
- [Sherry] Okay, beyond what's mandated by stars, where do you see the biggest area of investment for BBC implementation?
- [Erik] I think it depends a little bit on product line. In Medicare Advantage, I think we continue to see post-acute models of care being maybe an area of underinvestment by both plans and providers. It represents a part of the continuum that I think honestly represents probably the biggest near term savings that are available to these types of value-based care arrangements. I think post-acute isn't super well understood by acute care hospitals. I don't think it's well understood by most primary care physicians and I don't think MA plans totally understand what the levers are there. And I think there's a lot of opportunity in MA to get better at managing link to stay and skilled nursing, to manage people out of skilled nursing and into home health models and to manage people in the community. So in Medicare Advantage, I think that's where the biggest investment is. I think in Medicaid, I think it's in social determinant data collection and analysis and tying that to some of the health equity objectives in Medicaid. That is, again, I think this is a very new field even though we've been talking about it for a couple years, it's still very new. And I think that's where, if I were in a Medicaid managed care arrangement or I was taking on that level of risk, I would've been making significant investments in SDOH because I think that field hasn't been delimited yet. I think there's still a lot of variables that we probably don't understand very well that if we did it would give us a lot more insight into how to engage with the community and some of the community stakeholders like school clinics, churches, senior centers, community centers, YMCAs, where you can start to address some of the health inequities and actually start to inflect patient's care. So in those two product lines, those are the two areas where I find there to be a lot of fertile ground for farming.
- [Sherry] Okay, I know we're at the end of our session, but we've got one quick question. Why is patient satisfaction key to successful programs and what happens when the patient doesn't buy in?
- [Erik] Yeah, great question. Two things, I think come immediately to mind. The first is you wanna own the life. I mean, ultimately the coin of the realm in value-based care is owning the life and having that life as long as possible because you're gonna be making investments on behalf of those lives in population health and care management programs. And sometimes, the return on that investment is gonna require more than one benefit period. So keeping the patient happy and satisfied so they stay in your insurance product gives you a much longer runway in order to realize the return on some of those investments that you're gonna wanna make anyway. So I think that's the first reason patient satisfaction matters so much. I think the second reason it matters so much, and I sort of alluded to this maybe middle of the presentation, is that, you do want a lot of your patients actually to engage with their benefit plans and to engage more aggressively with their providers. And making that hard ultimately is going to result in worse health outcomes and higher spend. If it's just too much of a hassle to schedule a colonoscopy for particular individuals, then a lot of colonoscopies are gonna go undone and some of those are gonna result in cancer going down the line. Making it easy on the other hand, while it's gonna cost you a lot, it maybe may, it might prevent the occurrence of a real acute expensive episode 16 months from now. And I think patients are pretty smart and I think they know what easy looks like today because of their experiences in other product lines, not healthcare, but consumer, retail, airlines, banking, what have you. That all looks easy. Healthcare looks hard, and making it easy for them to engage with their benefits, I think will result in them being happier. You'll keep them longer and you'll ultimately have better outcomes.
- [Sherry] Well, thanks. That's the end of our questions. And I want to thank everybody for attending today's showcase session presented by Optum. I'd also like to thank the Optum team for a great presentation. Remember that today's session has been recorded and will be posted along with the slide deck and some additional information on the Value-Based Payment Showcase event page on the ACAP website under vendor showcases. Thanks, again.
Learn more from our experts about health care's most complex topics.
Related content

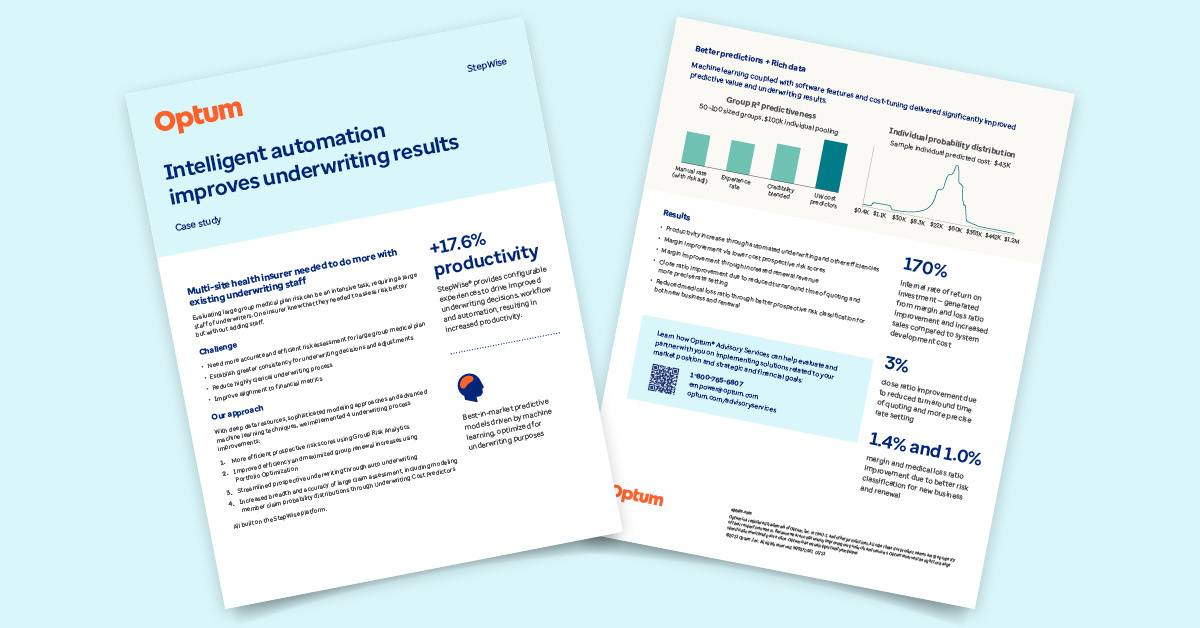
Transform underwriting with cutting edge technology