Data integrity is critical
It’s the age-old balancing act. Health care organizations have a finite number of dollars to spend across competing priorities while being under continuous pressure to reduce costs, improve health care quality and ensure all applicable regulatory requirements are satisfied.
For risk-adjusted populations, it’s important to consider how complete and accurate reporting of your health plan’s membership plays a role in this equation.
Most health plans are continuously implementing new or modifying existing cost-saving measures across almost every department. These initiatives may include medical management reviews, narrow networks or other targeted operational strategies. For risk adjustment, reducing costs may include cross-training teams to work on multiple lines of business or employing targeted analytics for certain programs like chart review.
We generally see risk adjustment programs advance as a health plan matures. For example, new health plan entrants may focus on retrospective chart reviews, while those that have been in the market longer often add in-office and in-home assessments. Whether the emphasis is on retrospective, prospective or a combination of both programs, the goal is to ensure accurate, complete and timely reporting of data.
Many plans have realized the impact of data integrity. Optum has found that incomplete encounter data accounts for a revenue loss of up to $63 per member per year.*
Encounter data quality is not only important for accurate and complete reporting; it can also help reduce costs, improve quality scores and have a positive impact on health care outcomes.
Start with submission data
While the models vary between Medicare Advantage, Affordable Care Act populations and Medicaid, the need for accurate, complete and timely data submissions are the hallmark of all three risk-adjustable populations.
With the last RAPS submission now in the rear-view mirror for most Medicare Advantage plans, the need for improved encounter data quality for Encounter Data System (EDS) submission requirements is even more critical.
Regardless of line of business, submissions data passes through multiple hands.
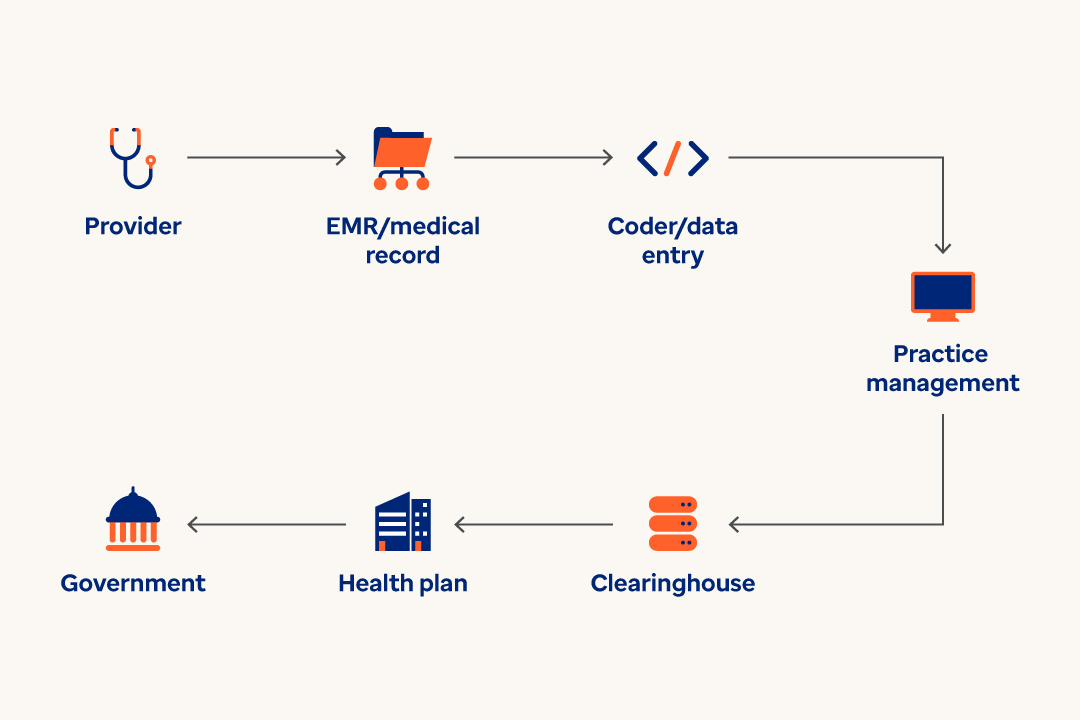
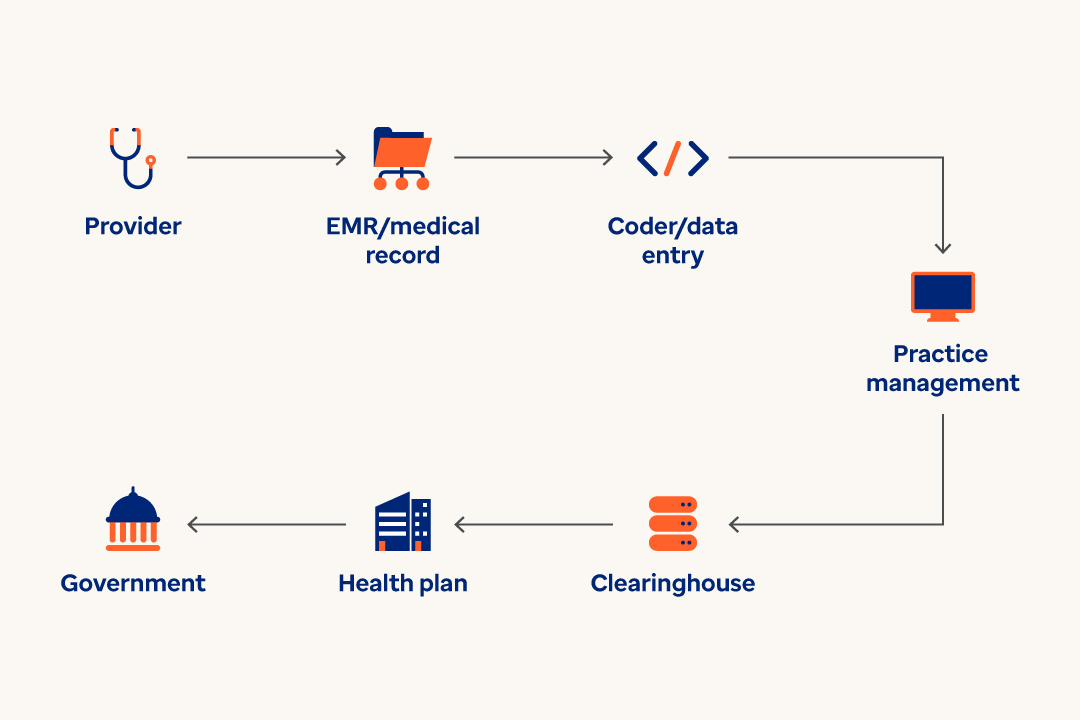
From providers, to clearinghouses, plans and ultimately to the appropriate government entity, there can be numerous hand-offs in the overall submission process — and from team to team within each entity. Each transition of the data represents data leakage risk. When encounter data is leaked, it becomes incomplete and inaccurate.
Health plan and provider collaboration
Whether in a payvider scenario or value-based contracting arrangement, provider organizations are taking on more risk and engaging in new and unique contracts with health plans. In the process, they’re becoming increasingly interested in end-to-end reconciliation with health plans.
With interests aligned, health plans are in a great position to discuss encounter data quality with their provider partners and engage further in reconciliation.
Data trends such as the number of diagnosis codes submitted per claim are another good leading indicator of a data integrity issue.
Monitoring these trends on an ongoing basis is important for identifying data quality changes. System implementations or upgrades can also inadvertently cause these changes, resulting in inaccurate revenue for your health plan.
Four takeaways on encounter data quality
As health plans look to improve their visibility into potential encounter data quality issues, here are the four key takeaways:
- Encounter data quality matters. The quality of encounter data that a health plan receives from providers through claims and encounters directly impacts data reporting and associated revenue. It also impacts cost and quality.
- Payer and provider partnership is a must. Health plans and providers need to work together to capture and report complete and accurate diagnosis data to reflect the true health status of their population. In turn, both health plans and providers benefit from improved insights into their populations — driving better health outcomes.
- Consider different perspectives. When thinking about capturing and reconciling encounter data, it is best to think about it two ways: 1) from the provider’s point-of-care to claims data billed to the health plan, and 2) from the health plan through submission to respective government entity.
- Continuously monitor. With ongoing audits, it’s always a great time to evaluate the quality of your encounter data to improve data throughput and program effectiveness.
Optum can help
Optum® Advisory Services has risk adjustment subject-matter experts and actuarial resources to help you optimize the quality of your encounter data. Whether you need assistance in developing end-to-end reconciliation processes and reports or simply want an objective review of your program and data quality, we are well positioned to partner with you to mitigate data leakage. The result is improved accuracy of your revenue, quality scores and the potential reduction of costs.
*Based on recovery of MA health plans engaged in the Optum® Data Leakage programs to capture diagnosis data that was documented at the point of care and inadvertently dropped prior to submission to CMS.


