Better, more efficient use of specialty drugs
Following specialty patients throughout their care is key to cost-effective use of high-cost drugs.
In the pharmacy benefits world, we typically think of non-adherence in terms of people not taking their medications as prescribed. It is that, but non-adherence also includes other aspects of care, including patient follow-up visits.1
Non-adherence has many causes. There may be practical barriers, such as the financial difficulties and the complexity of the therapy. There may also be issues in the patient’s life, such as cultural beliefs, alcohol use, depression, anxiety or reduced cognitive abilities.2
Regardless of why, non-adherence causes many problems. Overall, non-adherence to therapy leads to preventable hospitalizations and deaths and costs the U.S. health system half a trillion dollars every year.3
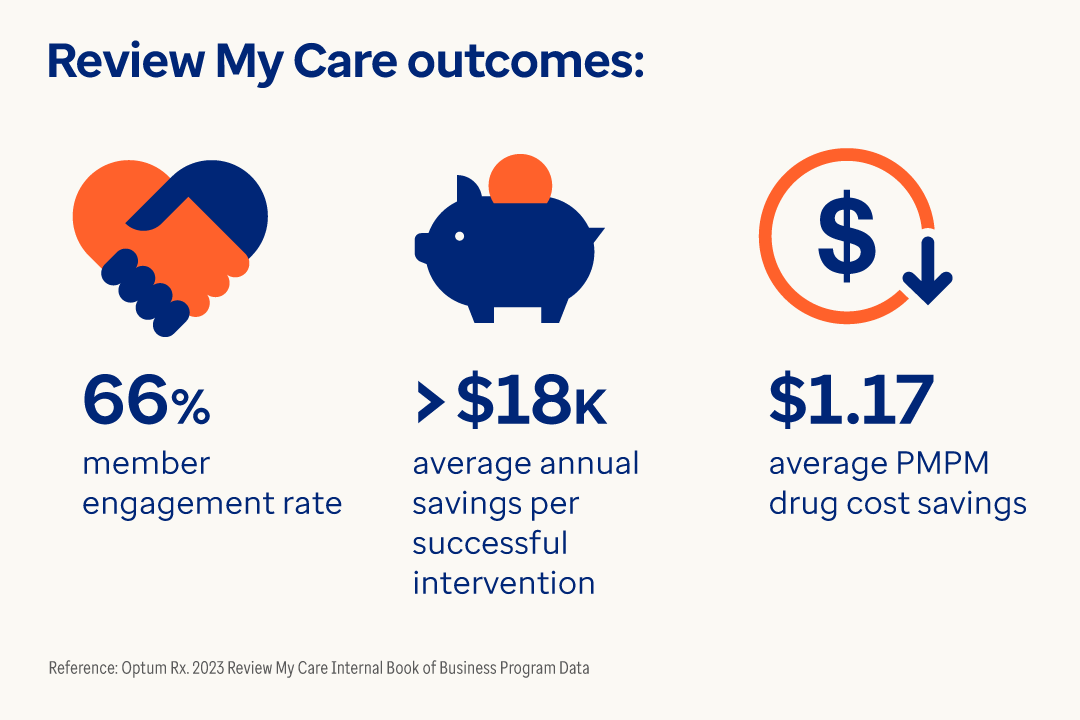
Patient follow-up for specialty drugs
Now let’s zero-in on specialty medicines. Specialty drugs are often high-cost, limited distribution medications that are used to manage rare, chronic and complex medical conditions.
These drugs require more intensive patient management, since patients may require financial assistance, dosing instruction and counseling.4 As such, adhering to a continuously monitored care plan becomes even more important.
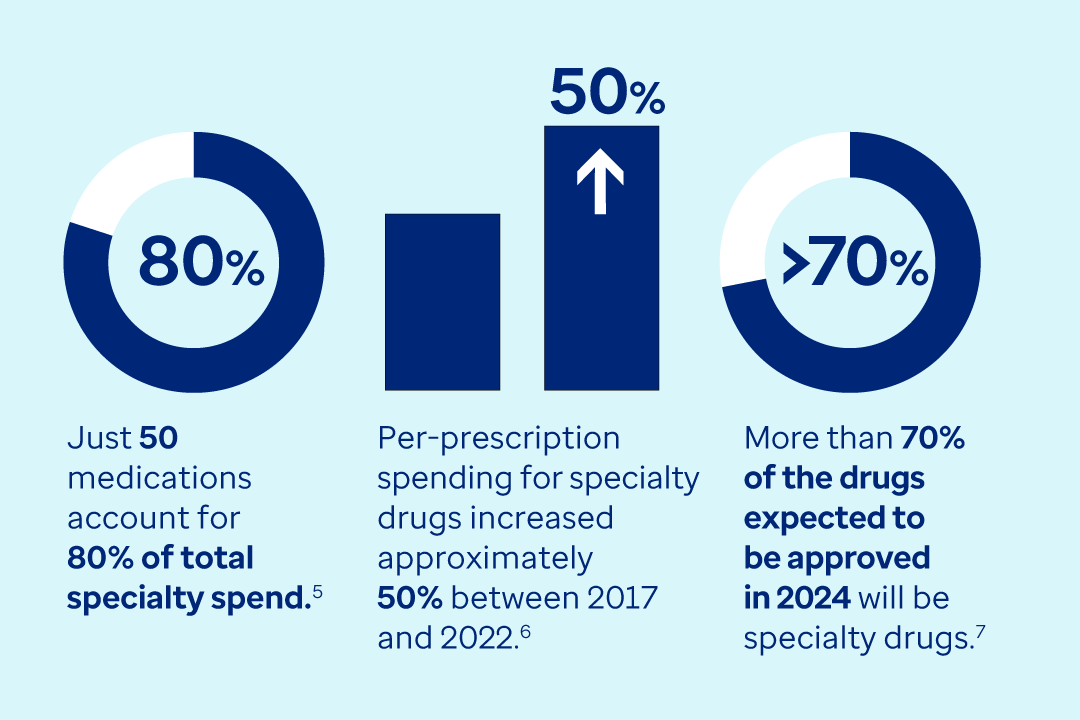
Specialty spending is high, getting higher
Proper management of specialty drugs is essential for a financially viable pharmacy benefit plan.