Build trust and measure outcomes to help increase patient access
Health care’s embrace of value-based care requires life sciences companies to create strategies that focus on patient outcomes. To secure access to a higher formulary tier or broaden access, manufacturers need to prove the value of their products to payers, whose own goals may include:
- Managing overall total cost of care
- Reducing uncertainty in financial estimates
- Sharing the risk associated with drugs whose real-life performance is still unknown
More targeted therapies often come to market with high price tags — but that doesn’t mean they can’t be cost effective. A treatment’s effects on patient prognosis, quality of life, productivity and more can all factor into its value versus the standard of care.
Value-based contracts (VBCs), also known as outcomes-based contracts (OBCs), are written agreements that offer an effective avenue to increase patient access and mitigate risk.
VBCs are built upon a foundation of real-world evidence (RWE) that provides information like patient and provider characteristics, treatment outcomes and market share. Value-based contracting also generates valuable evidence on the ongoing performance of a drug, acting as a great source of RWE themselves.
When life sciences organizations consider using value-based contracts, they need a partner that understands their needs, the market dynamics driving payer decisions and the complexities of clinical care. Optum experts work with manufacturers, payers and providers to:
- Find endpoints that are measurable and relevant to all stakeholders
- Build trust and understand multiple points of view
- Use real-world data and analytics to monitor and measure VBC outcomes
Explore health economic modeling
Translate a product’s clinical benefits into tangible and measurable economic benefits.
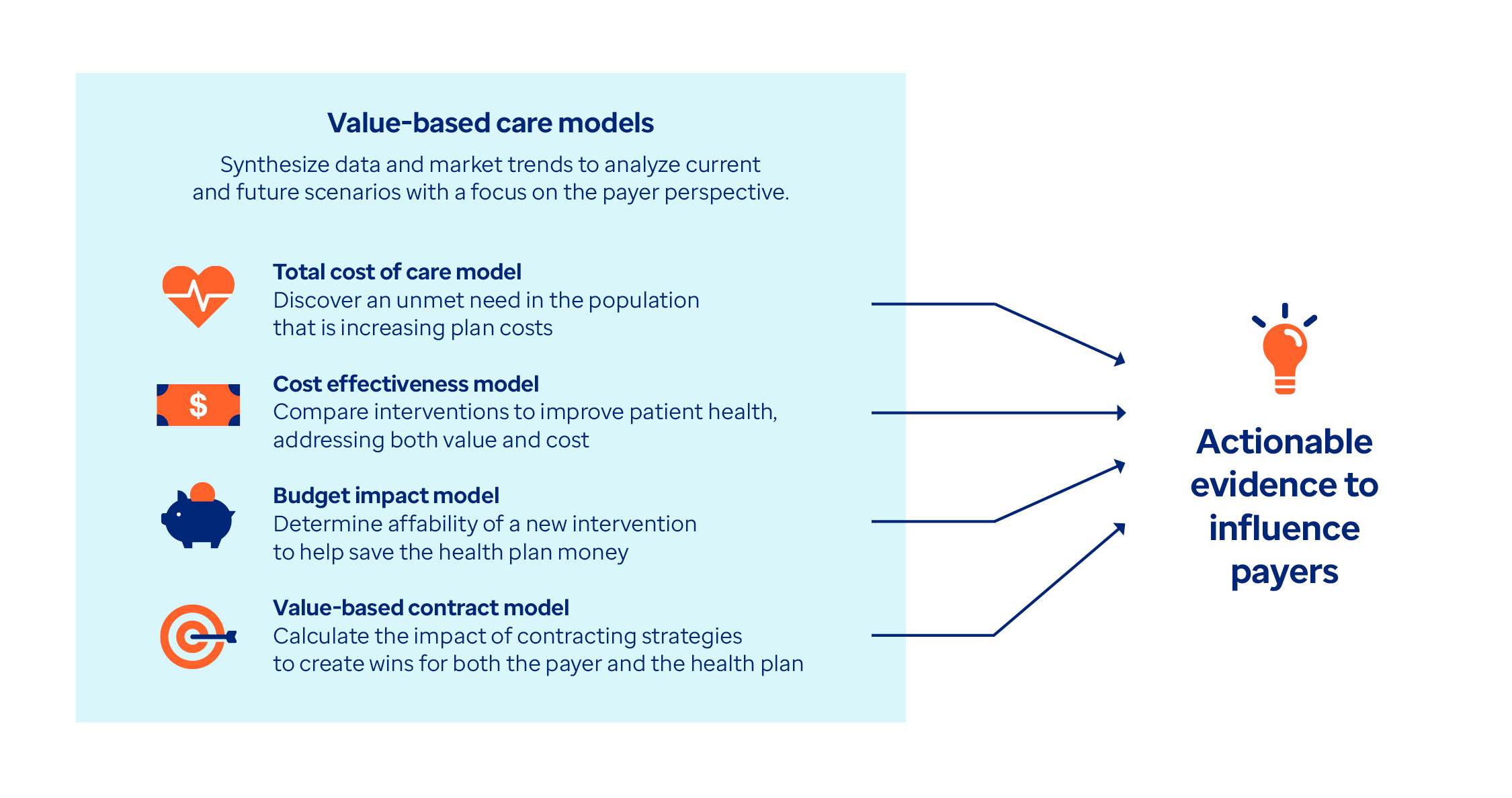
Health economic model types include total cost of care, cost effectiveness, budget impact and value-based contract models.
Leaders with deep domain expertise and industry knowledge
Optum experts dedicated to value-based contracting help stakeholders across the health system work together to support patient access.


Why Is Collaboration So Important in VBAs?
Leaders from Takeda, Optum Rx, and Optum Life Sciences collaborated to create value-based agreements (VBAs) to understand patient and client needs.
Integrating VBC approaches across phases of the product lifecycle
- Conduct literature review synthesis to understand current physician practice
- Understand clinical guidelines as well as payer orientation in these areas
- Fill knowledge gaps with payer, physician, and/or medical society leader interviews
- Assess the diagnostic journey and treatment pathway for patients
- Leverage machine learning and natural language processing (NLP) to create diagnostic algorithms when definitive ICD-10 codes are unavailable
Identify which outcome measures can be reliably captured in the real world to inform the outcomes-based contract design. Work with Optum to expand the outcomes that can be measured in a VBC, like:
- Pharmacy claims: adherence and medication switching
- Medical claims: procedures, inpatient events, total cost of care
- Chart review: disease progression, functional tests
- Patient surveys: patient-reported outcomes and long-term follow up
- Define the following through consulting engagement:
- Support the key themes for payer value story through real-world evidence (RWE)
- Define modeling objectives to create a total cost of care model, budget impact, and/or contract simulation
- Conclude with a payer and clinician summit that reviews past materials and provides guidance
Understand the effect of key patient demographics, disease severity, disease progression, treatment patterns and cost of therapy on total cost of care.
Apply patient journey insight and disease state total cost of care to test different scenarios for contracting:
- Different clinical thresholds
- Different payer types
- Different rebates values
- Performance vs. traditional rebate
- Develop a pre-launch information exchange deck and tools that help relay the critical product and disease state insights that are important to payers
- Use key drug information, RWE, outputs from disease and total cost of care model and payer strategies to develop a VBC framework
- Ensure VBC framework consists of drug value proposition as well as key information such as clinical outcomes measures, value milestones and consideration by payer book of business
- Leverage VBC data aggregation to support longitudinal patient or population-based programs
- Discover real-world clinical performance and financial risk exposure through the breadth of payer relationships brought together through Optum
Related resources

Toward Outcomes-Based Payments

Solve contract challenges for gene therapies

Reflections on PCMA's recent Annual Meeting

Supporting providers in the transition to VBC
Complementary solutions

Strengthen your value story with HEOR

Design, Pilot and Scale Engagement Programs
Take advantage of our connections to all parts of the health system.

Voice-to-Claim Research
The Optum® HEOR Primary Data Collection (PDC) team focuses on real-world evidence generation through primary and secondary data.



